
Dec 7, 2023 | Common Solutions, News
Platelet-Rich Plasma (PRP) for urine incontinence
In urology, platelet-rich plasma (PRP) for urine incontinence involves injecting platelet-rich plasma into the bladder and urethra walls, to heal outbreaks influenced by inflammatory processes. The growth factors in the platelets stimulate mucous regeneration and lesion repair.
Understanding Urinary Incontinence: A Common and Challenging Issue
Loss of bladder control, or urinary incontinence, is a common and frequently humiliating issue. The intensity varies from a slight leakage of pee when you cough or sneeze to an intense urgent urge to urinate that prevents you from reaching a bathroom in time.
Dispelling Myths: Aging Doesn’t Guarantee Urinary Incontinence
Though it occurs more often as people get older, urinary incontinence isn’t an inevitable consequence of aging. If urinary incontinence affects your daily activities, don’t hesitate to see your doctor.
Comprehensive Approaches to Urinary Incontinence Management
Sufferers of urinary incontinence experience a diminished quality of life due to the embarrassment and shame associated with the condition. Non-invasive approaches, such as the use of pads, external urine collection devices, behavioral modifications, and pelvic floor exercises, are commonly employed. Surgical options, such as suburethral sling procedures for women and various procedures for men, including injections, sling implantation, artificial urinary sphincter placement, constrictors, and stem cell therapy, are often necessary, particularly for postprostatectomy incontinence. However, some individuals with mild urinary incontinence may resist invasive surgical treatments. Minimally invasive alternatives like urethral bulking agent injections or stem cell therapies have been developed but are not yet established as simple and effective treatments.
Revolutionizing Treatment: Platelet-Rich Plasma (PRP) Therapy
Urinary incontinence, a prevalent and often distressing condition, has seen promising advancements in treatment modalities. Among these, Platelet-Rich Plasma (PRP) therapy has emerged as a novel and effective approach. PRP, derived from the patient’s own blood, is rich in growth factors that stimulate tissue regeneration and repair. In the context of urinary incontinence, PRP is thought to enhance the strength and integrity of the pelvic floor muscles and surrounding tissues, ultimately improving bladder control. This minimally invasive procedure has gained attention for its potential to address the root causes of incontinence and promote long-lasting relief.
Exploring the Regenerative Potential of Platelet-Rich Plasma (PRP)
The increasing popularity of autologous platelet-rich plasma (PRP) as a therapy for enhancing wound healing is notable. PRP, rich in growth factors and cytokines, is widely studied in trauma cases and experimental models. Its local application, combined with bone marrow-derived progenitor cells, has shown promise in tissue regeneration. PRP, derived directly from the patient’s blood, is considered superior to synthetic materials due to its lower risk of adverse effects.
PRP’s Role in Healing and Beyond: Insights from Recent Research
During wound healing, platelets release biologically active molecules, playing a crucial role in tissue regeneration. Recent research highlights the immunomodulatory effects of PRP on the inflammatory response, making it a valuable source of growth factors for improved healing. Additionally, PRP injections have demonstrated potential in alleviating neuropathic pain and improving symptoms in patients with interstitial cystitis/bladder pain syndrome.
Using PRP to improve Urethral Health: A Reasonable Method
Given PRP’s regenerative potential, injecting it into the urethral sphincter to enhance muscle bulk and urethral resistance appears rational. Autologous PRP, lacking antigenicity, is considered safe and has been proven effective in facilitating wound healing and treating interstitial cystitis.
Realizing the Benefits: Transforming Lives with PRP Therapy
Benefits
-Decreased urinary incontinence in a week or two.
-Improvement in confidence when amongst friends.
Sep 13, 2022 | Cystoscopy, News
Cystoscopy Bladder Scope Test
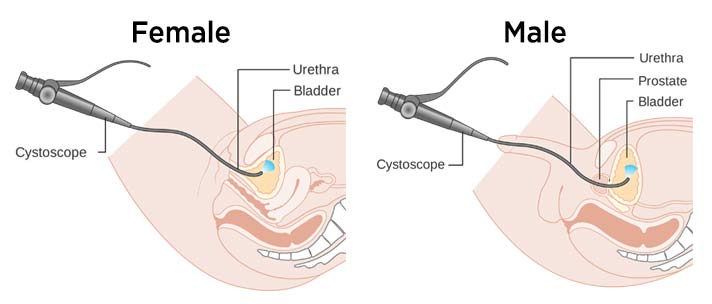
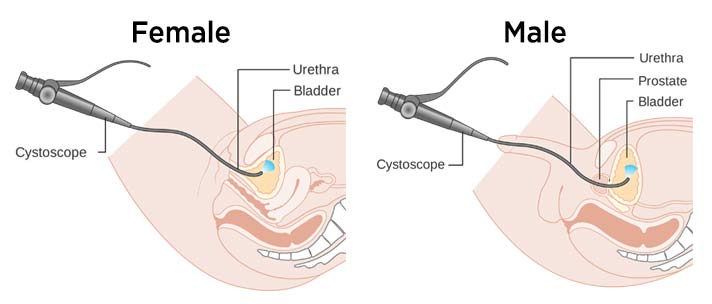
What is a cystoscopy?
A cystoscopy is a test to check the health of your urethra and bladder. You might also hear it called a cysto-urethroscopy or, more simply, a bladder scope.
Cystoscopy is a procedure that uses an instrument called a Cystoscope to look at the lining of the bladder (the area where urine is stored), the opening of the ureters (the tubes that connect the kidneys to the bladder), and the urethra (the tube that runs from the bladder to the outside of the body).
How Does the Test Work?
The Cystoscope is a thin instrument with a lens at the end so the inside of the bladder can be seen. It is usually attached to a television screen. The procedure is an outpatient test, which means you can get it at your doctor’s office, or clinic and hospital the same day. It may or may not require anesthesia, and it lasts for approximately 10-15 minutes.
The doctor inserts a tube into your urethra.
Who might need a cystoscopy?
The urologist may recommend a cystoscopy if you experience:
• Bladder control issues, such as urinary retention (being unable to empty the bladder all the way) or incontinence (Leaking or peeing when you aren’t trying, or pain when you pee)
• Bladder stones.
• Blood in urine (hematuria).
• Frequent urinary tract infections (UTIs), to find the cause of frequent urinary tract infections
• Painful urination (dysuria).
• Difficulty in passing urine – which may be due to prostate enlargement or a narrowing (stricture) of the urethra.
• Diagnose an enlarged prostate
• Diagnose bladder diseases like bladder cancer, that needs treating (including some early cancers)
• Bladder stones, and bladder inflammation (cystitis)
• Treat conditions: Removal of small tumors through the cystoscopy
• To monitor progress of conditions: Some patients have a routine cystoscopy after treatment for a bladder tumor.
What to Expect Before the cystoscopy
•No special preparations are required.
•You may eat, drink, and take your medication as usual.
What to Expect during the cystoscopy
1. You will remove any clothing, jewelry, or other objects and you will be given a gown to wear
2. You’ll lie down on an exam table on your back with your knees up and spread apart
3. You might get an IV (intravenous) line for sedative medications: if the cystoscopy is under anesthesia (in the hospital)
4. This will make you sleepy and not feel pain during the cystoscopy. In this case, your heart rate, blood pressure, breathing, and blood oxygen level will be watched during the procedure.
5. The cystoscope is inserted through the urethra into the bladder with a liquid or gel anesthetic is used during the insertion of the cystoscope to minimize pain or discomfort (In the Clinic).
6. If you’re a man, the opening is at the end of your penis.
7. If you’re a woman, it’s just above your vagina.
8. The test lets your doctor check the complete length of your urethra and the bladder for polyps, narrow areas called strictures, abnormal growths, and other problems.
9. Water or saline is infused through the cystoscope into the bladder. While the fluid fills the bladder, the wall of the bladder become stretched so the urologist can see clearly.
10. The Doctor will ask you how it feels when your bladder is full.
11. In case of an abnormal tissue is seen, the doctor will use the cystoscope to cut a small piece to send it to the lab for analysis. They’ll call this a biopsy or tissue sample.
12. Discomfort and pain during cystoscopy:
• You may feel discomfort when the cystoscope goes into the urethra and bladder; a strong need to pee when your bladder gets full.
• You may feel a slight squeeze if the doctor takes a tissue sample (Biopsy)
13. At the end of the procedure, the cystoscope is removed and you can empty your bladder.
What to Expect After the Cystoscopy
• You should drink plenty of fluids to flush out your bladder.
• You may experience some of the following:
• Blood-colored urine. This should go away in 2 to 3 days.
• Burning sensation with urination for 2-3 days
• Discomfort with urination for 2-3 days
Possible Complications of cystoscopy
• Infection
• Bleeding
• Urinary retention due to irritation and swelling from the procedure
• Bladder perforation (poking a hole in the bladder with the cystoscope)
When to contact your doctor or the clinic
if you notice any of the following after the cystoscopy:
• Shaking Chills or Fever: Sign of infection
• Bright red urine
• Peeing less than usual
• Worsening pain or discomfort on urination
• Lower back pain
• An inability to urinate

Jun 17, 2021 | Common Solutions
Overactive bladder diagnosis and treatment are very necessary to continue your life without depression and stress.
Overactive Bladder Diagnosis
We can have the same symptoms of OAB in :
-Urinary tract infection.
-BPH.
-Bladder cancer.
-Interstitial cystitis, prostatitis.
When you have these symptoms you should visit your urologist who will:
-Ask about your symptoms and your medical history.
-Do a physical exam for your abdomen, your rectum, and the organs in your pelvis.
-Bladder Diary: The patient should note how many times he goes to the bathroom and when he leaks urine; the bladder diary helps you track: when and how much fluid you drink, when and how much you urinate in 24 hours, how often you have the urgency feeling to urinate, when and how much you leak urine.
Other Tests
-Urine test: Your doctor will require a urine analysis and urine culture to determine if there’s a urine infection.
-Bladder scan: This ultrasound imaging shows how much urine is still in the bladder after you go to the bathroom.
-If there is any doubt about the diagnosis, the urologist required a cystoscopy or urodynamic testing.
Overactive Bladder treatment
Overactive bladder can interrupt your social life, but there are ways to combat the problem.
Natural Treatment for Overactive Bladder

-Bladder training: This type of training helps the patient to control the urge of urinating; he will able to control himself.
-Pelvic floor exercises: Called Kegels exercises; you tighten, hold, and then relax the muscles that you use to start and stop the flow of urination.
Drugs for Overactive Bladder
In the overactive bladder, we have contraction of the muscles in the bladder wall at the wrong time. A group of drugs called anticholinergics help by blocking the nerve signals related to bladder muscle contractions; these medications increase bladder capacity and decrease the urge to urinate.
Anticholinergic drugs include:
Darifenacin (Enablex)
Fesoterodine (Toviaz)
Oxybutynin (Ditropan, Ditropan XL, Gelnique, Oxytrol)
Solifenacin (Vesicare)
Tolterodine (Detrol, Detrol LA)
Trospium (Sanctura)
These drugs have several side effects:
-dry eyes
-dry mouth
-Constipation
To relieve dry mouth it is necessary to drink small amounts of water (because large amounts can worsen the symptoms of the overactive bladder) and suck a sugar-free candy; the doctor will recommend eye drops to relieve dry eyes and a diet rich in fiber for constipation.
Bladder injections
OnabotulinumtoxinA, also called Botox, is a protein injected in small doses directly into the bladder to relax the muscles. The effect of this protein lasts for 6 months so repeated injections are necessary.
Side effects of Botox injection: urinary tract infections and urinary retention.
Nerve stimulation
Helps to treat an overactive bladder by adjusting nerve messages from the brain to the bladder.
We have 2 types of nerve stimulation:
-Sacral nerve stimulation (SNS)
-Percutaneous tibial nerve stimulation (PTNS)
Follow the link for more information about nerve stimulation.
Surgery
Surgery is required for people with severe symptoms who don’t respond to other treatments.
We have 2 types of surgeries:
-Surgery to increase bladder capacity by using pieces of your bowel to replace a portion of your bladder. This surgery is required only in cases of severe urge incontinence that doesn’t respond to any other treatment.
-Bladder removal: This procedure is the last solution of severe overactive bladder and consists of removing the bladder and surgically constructing a replacement bladder (neobladder) or an opening in the body to attach a bag on the skin to collect urine.
Some TIPS to prevent an overactive bladder
-Maintain a healthy weight.
-Do physical activities and exercises.
-Reduce your consumption of caffeine and alcohol.
-Stop smoking: smoking is irritating to the bladder muscle.
-Treat your chronic conditions, such as diabetes, that might lead to overactive bladder symptoms.
-Do Kegel exercises for the pelvic muscles.

Jun 7, 2021 | Common Solutions
Urinary tract infections in women
Women have a high risk (over 50 percent) of developing a urinary tract infection (UTI), especially in the case of pregnancy; where a urine test is required even if there are no symptoms because a urine infection can be dangerous for both maternal and infant health.
Causes
The essential cause is the bacterium Escherichia coli (E. coli), found in the digestive system. Chlamydia and mycoplasma bacteria can cause infection in the urethra, but not in the bladder.
When the infection is located:
-In the bladder: cystitis.
-In the urethra: urethritis.
-In the kidney: pyelonephritis.
The ureters are very rarely the site of infection.
Risk factors
-Sexual intercourse with multiple or new partners (especially Chlamydia and gonorrhea).
-Diabetes.
-Bad personal hygiene.
-Problems emptying the bladder completely.
-A urinary catheter.
-Inability to control bowel movements.
-Blocked flow of urine.
–Kidney stones.
-Menopause.
–Pregnancy.
-A procedure aimed at the urinary tract.
-A suppression of the immune system.
-Immobility for a long period.
-Using spermicides and tampons.
-Take a lot of antibiotics, which can destroy the natural flora of the bowel and urinary tract.
Symptoms
Common symptoms of a UTI include:
-Urinate frequently in small quantities.
-Blood in the urine.
-Bad smell of urine.
-Pain when urinating.
-Nausea and vomiting.
-Muscle aches and abdominal pains.
-In case of Cystitis: low fever, pressure, and cramping in the abdomen and lower back.
Complications
Some upper UTIs can lead to serious problems; recurrent or non-treated kidney infections can cause permanent damage.
I the case of pregnancy, kidney infections can lead to premature delivery or to low birth weight.
Read more





 Robotic surgery
Robotic surgery Laparoscopic surgery
Laparoscopic surgery Prostate Laser surgery
Prostate Laser surgery Stone Laser surgery
Stone Laser surgery Sexual Health
Sexual Health Weight Loss Clinic
Weight Loss Clinic