Rezum Water Vapor Therapy The Best Choice For BPH
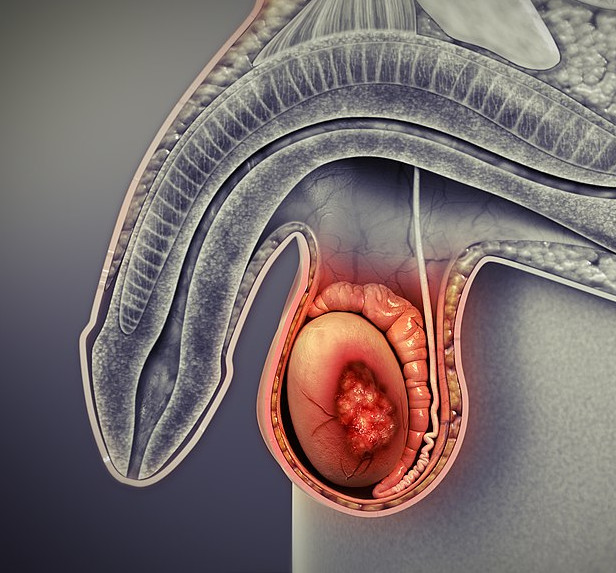
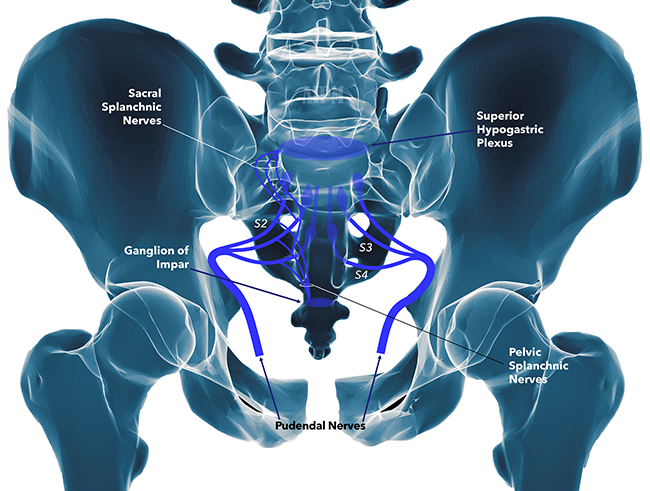
Rezum Water Vapor Therapy Why is Rezum Water Vapor Therapy the best choice? Rezum Water Vapor Therapy is considered an effective choice for several reasons, particularly for men suffering from benign prostatic hyperplasia (BPH), or an enlarged prostate. Here are some key benefits that make Rezum a favorable option:...