Obesity & Weight Loss

Weight Loss procedures There are several weight loss procedures that can be performed depending on the individual’s needs and medical condition. 1-Sleeve gastrectomy Obesity is a chronic condition in which there is a high amount of fat in the body. It is defined as a Body Mass Index (BMI) of 30 to 34.9 and extreme […]
Female Infertility

What is female infertility? Female infertility can be discussed when a woman is unable to conceive a pregnancy after trying for at least one year without using any form of contraception. In some cases, female infertility can also refer to a woman’s inability to carry a pregnancy to term, resulting in miscarriages or stillbirths. Other […]
5 Minutes Prostate Surgery With Our Rezum Expert Dr. Fouad Khoury
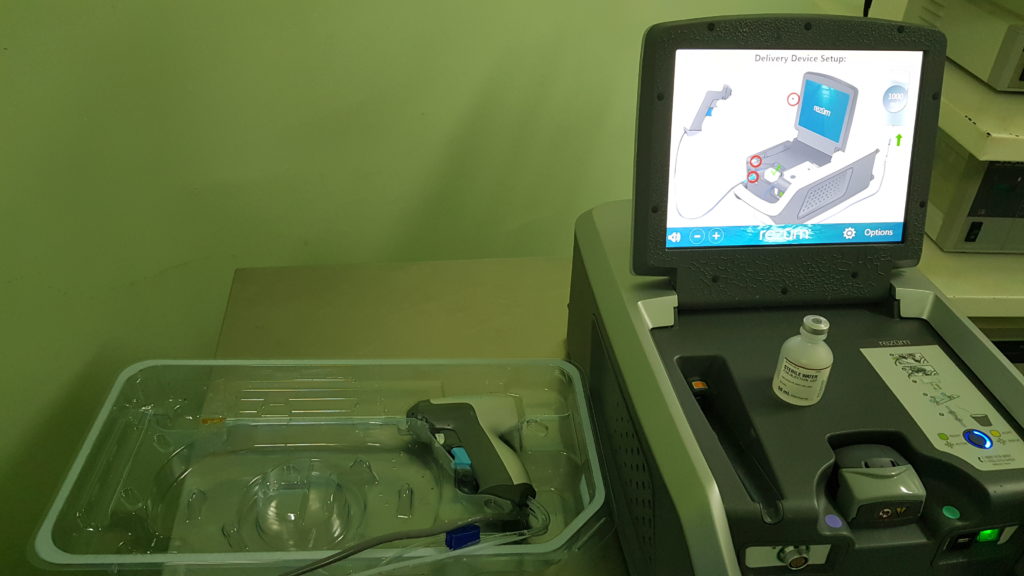
52 years old male patient: 45 gr prostate with failure to improve symptoms on medical treatment. Taking into consideration the patient’s age and sexual activities; he was insisting on undergoing a procedure to relieve his symptoms while preserving EJACULATION. A 5 minutes prostate procedure (REZUM) as shown in the video, recently promoted by The […]
Facts about bladder prolapse in Lebanon

Bladder Prolapse What’s bladder prolapse? A cystocele or a prolapsed bladder occurs when ligaments that hold your bladder up and the muscle between a woman’s vagina and bladder are weak; for this reason, the bladder will fall into the vagina. There are three grades of cystocele: – Grade 1: The bladder falls only a […]
Maintenance Therapy For Bladder Cancer
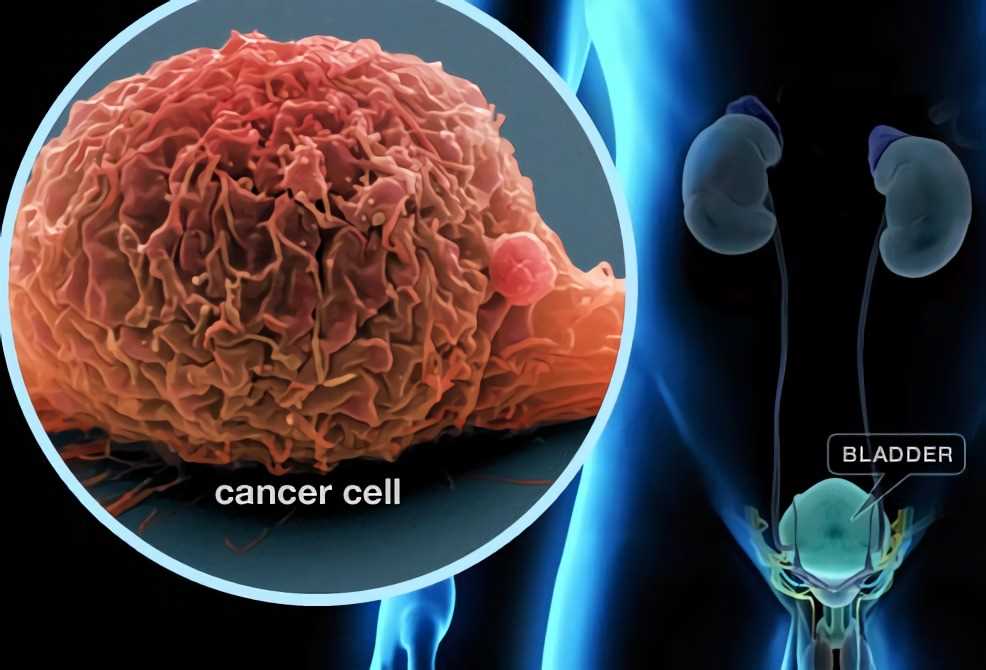
Maintenance Therapy For Bladder Cancer … What is the role of BCG? Bladder cancer can come back; for this reason, the patient needs follow-up tests for years after finishing the treatment. The best follow-up treatment is the BCG: Bacillus Calmette-Guérinthat used since 1920 to attenuated the action of the tubercle bacilli that causes tuberculosis. The […]
Diagnosis and Treatment for Bladder cancer

How to diagnosis Bladder cancer? There are many tests that help to diagnose bladder cancer. – Cystoscopy: This procedure is required to identify and diagnose bladder cancer. A cystoscope is inserted under local or general anesthesia into your bladder from the urethra to view the inside of the bladder and take a Biopsy that will […]
Facts About Bladder Cancer in Lebanon

Bladder Cancer Definition of the Bladder : The bladder is an empty muscular organ that stores urine until it is discharged out of the body through the urethra, and which is located in your lower abdomen. Where is bladder cancer located? Bladder cancer begins in the cells of the bladder lining, most commonly in the […]
Penile Prosthesis the BEST surgical treatment for ED in Lebanon
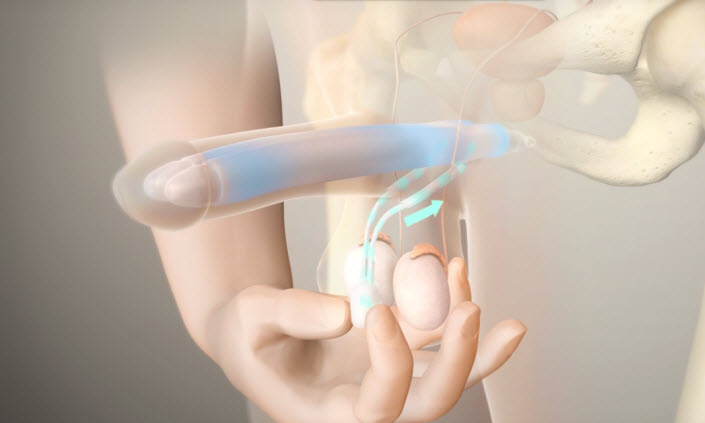
Penile prosthesis Definition A penile prosthesis or Penile Implant is the best surgery that helps men with erectile dysfunctions when other treatments failed. This procedure involves placing a prosthetic device or penile implant inside the penis and scrotum; so the patient can get a sufficient erection for sexual activities. And it lasts for 45 minutes […]
Laparoscopic Radical Nephrectomy-14 cm tumor
This movie features a challenging laparoscopic left radical nephrectromy for a huge tumor compressing the aorta and overlying the kidney pedicle. The procedure was successfully performed by Dr. Fouad Khoury with minimal blood loss and optimal post-operative results.
First Complex Robotic Assisted Partial Nephrectomy
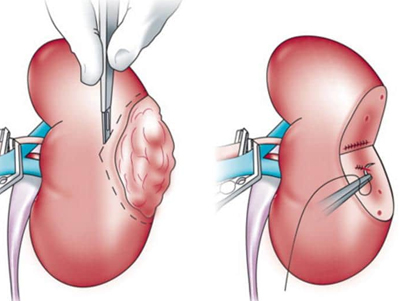
Robotic Assisted Partial Nephrectomy What is Robotic Assisted Partial Nephrectomy? Robotic partial nephrectomy surgery consists of removing a part of a kidney, to treat cancer by preserving as much healthy kidney tissue as possible. Who needs a robotic partial nephrectomy? -Patient with small kidney tumor (<4 cm in size). -Patient with risk of kidney […]
