Revolutionizing Treatment: Platelet-Rich Plasma (PRP) for urine incontinence

Platelet-Rich Plasma (PRP) for urine incontinence In urology, platelet-rich plasma (PRP) for urine incontinence involves injecting platelet-rich plasma into the bladder and urethra walls, to heal outbreaks influenced by inflammatory processes. The growth factors in the platelets stimulate mucous regeneration and lesion repair. Understanding Urinary Incontinence: A Common and Challenging Issue Loss of bladder control, […]
Understanding STDs

Sexually transmitted diseases (STDs) Sexually transmitted diseases (STDs) are a common concern for sexually active individuals. These infections can affect anyone, regardless of age, gender, or sexual orientation. While prevention is crucial, knowing when to consult a urologist for STD-related concerns is equally important. In this blog, we will discuss STDs, their symptoms, and […]
Pudendal Nerve Entrapment
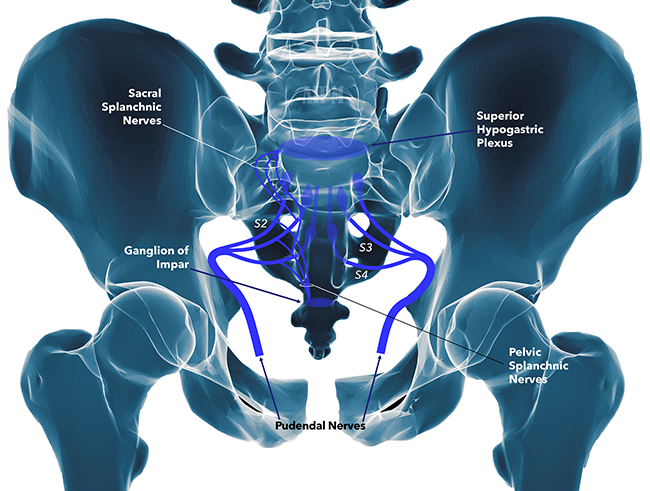
Introduction Within the realm of urology, many conditions are known to cause discomfort and distress to patients. One often overlooked but significant source of urological symptoms is pudendal nerve entrapment (PNE). PNE occurs when the pudendal nerve, responsible for sensory and motor functions in the pelvic region, becomes compressed or irritated. In this blog post, […]
Female Infertility

What is female infertility? Female infertility can be discussed when a woman is unable to conceive a pregnancy after trying for at least one year without using any form of contraception. In some cases, female infertility can also refer to a woman’s inability to carry a pregnancy to term, resulting in miscarriages or stillbirths. Other […]
Facts About Gout
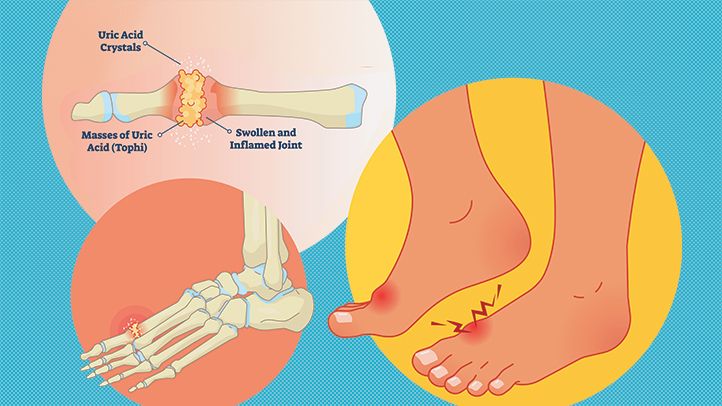
Gout What is Gout? Gout is a form of arthritis that causes sudden attacks of pain, redness, and tenderness in joints; especially the joint at the base of the big toe. Gout occurs when your body has extra uric acid; so urate crystals accumulate in joints, causing inflammation and intense pain. A crisis usually develops […]
Blood in urine!
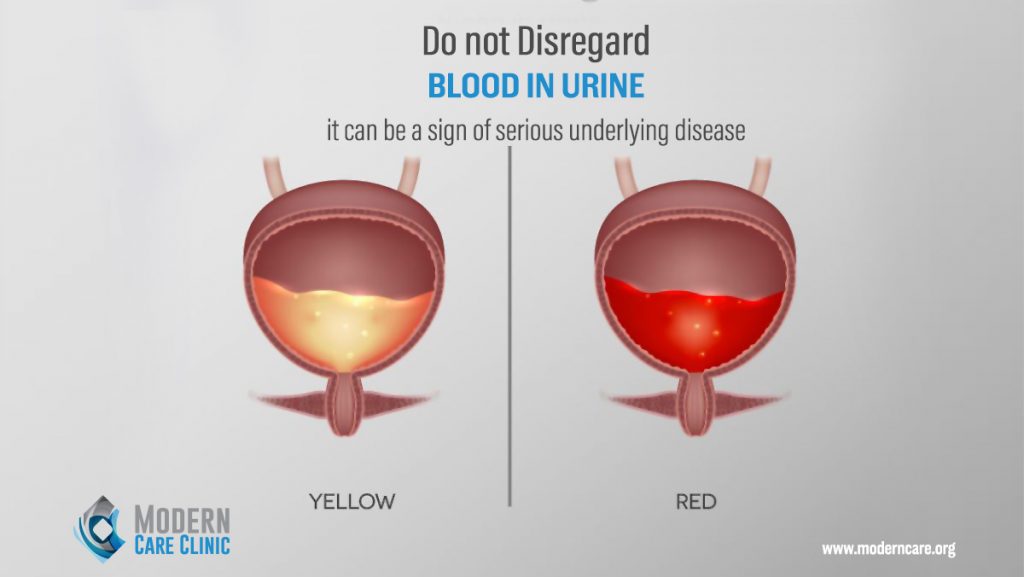
Hematuria Seeing blood in urine should never be ignored; because it can be a sign of a serious medical problem. It is the most common sign of bladder cancer that is usually painless, the urine color might change to orange, bright red, or brown. What is hematuria? Hematuria is the presence of blood cells in […]
Facts about bladder prolapse in Lebanon

Bladder Prolapse What’s bladder prolapse? A cystocele or a prolapsed bladder occurs when ligaments that hold your bladder up and the muscle between a woman’s vagina and bladder are weak; for this reason, the bladder will fall into the vagina. There are three grades of cystocele: – Grade 1: The bladder falls only a […]
Male Infertility
How is male infertility diagnosed? Diagnosis starts with a physical examination to evaluate your general state of health and identify any physical problems that may have consequences on your fertility. The doctor required the presence of the two partners and some tests: Semen Analysis Semen analysis is a routine lab test that helps to determine: […]
NO SPERM… MALE INFERTILITY!

Male Infertility Nearly 1 in 7 couples is infertile, which means there is no pregnancy even though they’ve had frequent, unprotected sexual intercourse for a year or longer. The male factor can be the cause of infertility, and this can lead to a stressful relationship. When to see a doctor? If no pregnancy after a […]
Overactive Bladder

Overactive bladder diagnosis and treatment are very necessary to continue your life without depression and stress. Overactive Bladder Diagnosis We can have the same symptoms of OAB in : -Urinary tract infection. -BPH. -Bladder cancer. -Interstitial cystitis, prostatitis. When you have these symptoms you should visit your urologist who will: -Ask about your symptoms and […]
