Rezum Water Vapor Therapy The Best Choice For BPH

Rezum Water Vapor Therapy Why is Rezum Water Vapor Therapy the best choice? Rezum Water Vapor Therapy is considered an effective choice for several reasons, particularly for men suffering from benign prostatic hyperplasia (BPH), or an enlarged prostate. Here are some key benefits that make Rezum a favorable option: 1-Minimally Invasive: Rezum is a […]
The Magic of PRP Therapy for Erectile Dysfunction

PRP Therapy for Erectile Dysfunction: A Revolutionary Approach Erectile dysfunction (ED) is a common condition affecting millions of men worldwide. Traditional treatments, such as medications and lifestyle changes, have been effective for many, but not all. For those seeking alternative or complementary therapies, Platelet-Rich Plasma (PRP) therapy is emerging as a promising option. What […]
Revolutionizing Treatment: Platelet-Rich Plasma (PRP) for urine incontinence

Platelet-Rich Plasma (PRP) for urine incontinence In urology, platelet-rich plasma (PRP) for urine incontinence involves injecting platelet-rich plasma into the bladder and urethra walls, to heal outbreaks influenced by inflammatory processes. The growth factors in the platelets stimulate mucous regeneration and lesion repair. Understanding Urinary Incontinence: A Common and Challenging Issue Loss of bladder control, […]
Learn about Cystoscopy!
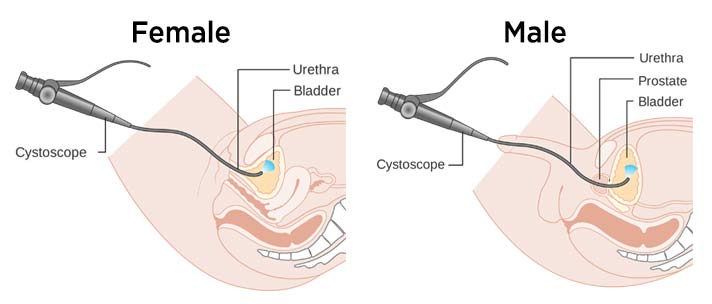
Cystoscopy Bladder Scope Test What is a cystoscopy? A cystoscopy is a test to check the health of your urethra and bladder. You might also hear it called a cysto-urethroscopy or, more simply, a bladder scope. Cystoscopy is a procedure that uses an instrument called a Cystoscope to look at the lining of the bladder […]
Best Prostate Treatment in Lebanon
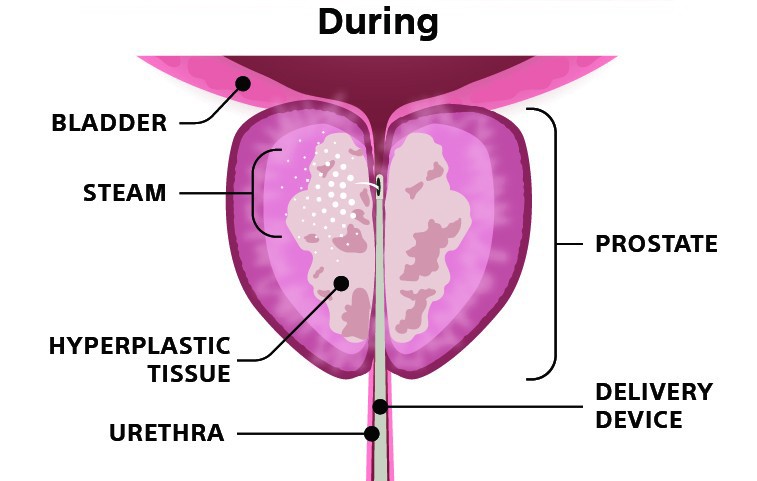
Prostate treatment in the Middle East / Lebanon Dr. Fouad Khoury discussing the most innovative prostate surgeries including minimally invasive transurethral water vapor therapy (Known as REZUM). Benefits of water vapor therapy : – 5 to 10 minutes procedure -Preservation of ejaculation -Preservation of sexual function – Done under local anesthesia – Same day procedure […]
Diabetes expert in Lebanon – 13 Easy Tips to Apply

Diabetes Tips to Apply 1. Tips to decrease your triglyceride level When we speak of increased cholesterol levels, it doesn’t always mean one thing. In fact, “total cholesterol” is defined as the sum of the good cholesterol (HDL), the bad cholesterol (LDL) and triglycerides. The danger to the heart and vessels come from either […]
Diabetes advice in Lebanon – Surprising Info in 2021

Advice for patients living with Diabetes 1. Your small blood vessels are at risk if your sugar levels are not at target! High sugar levels affecting the small vessels include damage to the retinal vessels, the small vessels of the kidney and the distal vessels of the nerves. Uncontrolled diabetes, whatever type it is, may […]
Magnifique Traitement du prolapsus genitourinaire

PALAIS DES CONGRÈS DE PARIS, 20 Novembre 2019
Bladder prolapse expert | Dr Fouad Khoury

Dr Fouad Khoury discussing minimally invasive approach to repair pelvic organ prolapses such as cystocele and rectocele. The repair can be done either through a laparoscopic or robotic approach with a success rate higher than 90 percent when done in expert hands.
Premature ejaculation

Premature ejaculation can be a frustrating problem for you and your partner.
