Female Infertility

What is female infertility? Female infertility can be discussed when a woman is unable to conceive a pregnancy after trying for at least one year without using any form of contraception. In some cases, female infertility can also refer to a woman’s inability to carry a pregnancy to term, resulting in miscarriages or stillbirths. Other […]
Male Infertility
How is male infertility diagnosed? Diagnosis starts with a physical examination to evaluate your general state of health and identify any physical problems that may have consequences on your fertility. The doctor required the presence of the two partners and some tests: Semen Analysis Semen analysis is a routine lab test that helps to determine: […]
NO SPERM… MALE INFERTILITY!

Male Infertility Nearly 1 in 7 couples is infertile, which means there is no pregnancy even though they’ve had frequent, unprotected sexual intercourse for a year or longer. The male factor can be the cause of infertility, and this can lead to a stressful relationship. When to see a doctor? If no pregnancy after a […]
Hurry up to treat varicoceles!
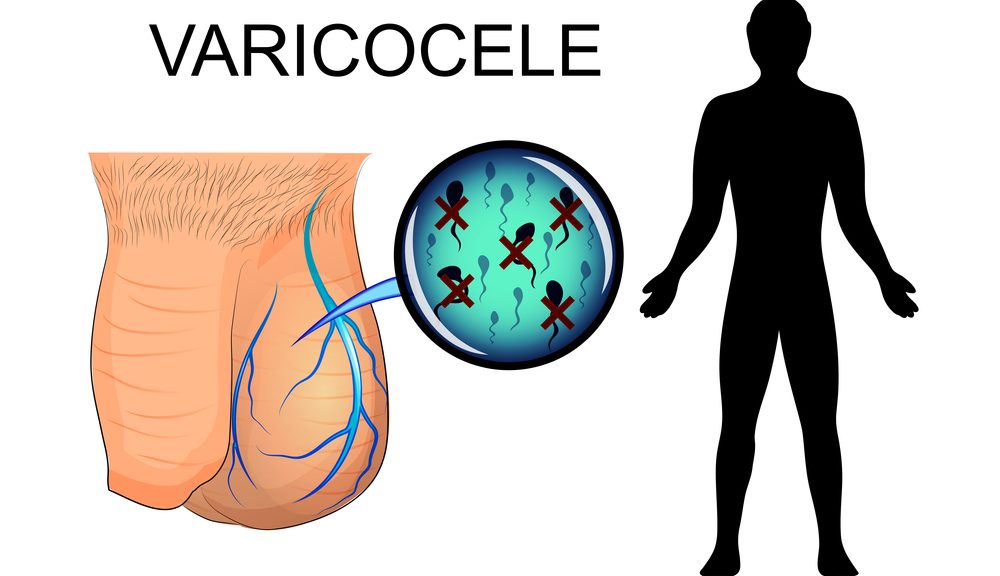
Varicoceles What are varicoceles? Varicoceles are when veins called pampiniform plexus become enlarged inside your scrotum (the sac that protects and holds the testicles). About ten to fifteen males out of one hundred have varicocele; it is like getting a varicose vein in your leg. This condition is most common in young men; and affects […]
Medical Tourism
Medical Tourism Travel to another country for medical care. Tell Me More Request For Healthcare https://moderncare.org/wp-content/uploads/2022/01/medical_tourism_en_sub.mp4 Medical Tourism can be defined as the process of traveling outside the country of residence for a short period of time for the purpose of receiving medical care. Many people find their comfort in consulting doctors in other countries, […]
Ask An Expert
Ask One Of OurMedical Experts Consult The Right People Check Frequently Asked Questions Call us +961 76 88 76 76 [email protected] Visit the Clinic Main Restaurant’s StreetAntelias, Lebanon The well-being of each patient is our goal, we do our best to ensure that our patients benefit from all our services. Schedule a Consultation Some patients […]
Let’s Know About Urinary Tract Infections In Men

Urinary Tract infections in Men What is a urinary tract infection? A urinary tract infection (UTI) is an infection that affects any part of your urinary system (kidneys, ureters, bladder, and urethra). There are 2 types of UTI: -Upper tract: in the ureters or kidneys. -Lower tract: in the bladder, urethra, or prostate in men. […]
