The Impact of Untreated STDs on Male Fertility and Urological Health
Many men in Lebanon might not realize how common STDs are or the silent damage they can do.
It’s a topic often whispered about, but its real-world consequences are serious.
We want to talk openly about The Impact of Untreated STDs on Male Fertility and Urological Health.
Ignoring these infections isn’t just a short-term issue; it can lead to long-lasting problems that affect your ability to have children and your overall urinary system health.
The Link Between STDs and Male Fertility
Direct Damage to Sperm and Reproductive Organs
Untreated STDs can cause inflammation and scarring that directly harm the reproductive system.
This isn’t just about feeling sick; it’s about physical damage.
Here’s how STDs can affect your fertility:
- Epididymitis: This is inflammation of the epididymis, the coiled tube behind the testicle that stores and carries sperm.
Chlamydia and gonorrhea are common culprits, leading to pain, swelling, and potential blockages. - Orchitis: Inflammation of the testicles themselves.
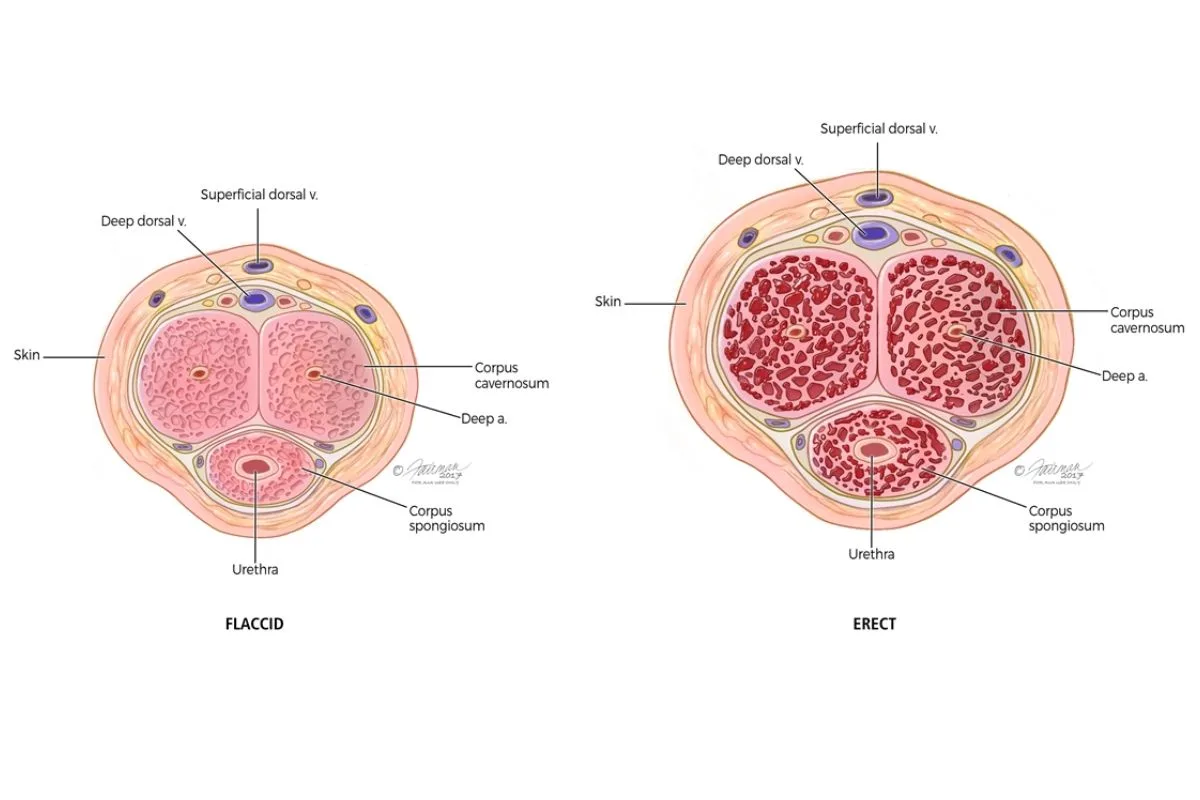
While less common as a direct STD complication, severe epididymitis can spread, impacting sperm production. - Urethritis: Inflammation of the urethra, the tube that carries urine and semen out of the body.
This can lead to discomfort and, if chronic, scarring that might affect semen flow. - Semen Quality: Infections can directly impair sperm count, motility (how well sperm move), and morphology (sperm shape).
This makes it harder for sperm to reach and fertilize an egg.
Beyond Fertility: Urological Health Risks
Chronic Infections and Blockages
The urinary tract and reproductive system are closely linked, so an infection in one can easily spread to the other.
Untreated STDs can cause a range of urological problems.
- Prostatitis: Inflammation of the prostate gland.
Some STDs can lead to chronic bacterial prostatitis, causing pelvic pain, painful urination, and ejaculation issues.
You can learn more about prostate health on our prostate category page. - Urethral Strictures: Repeated inflammation from STDs can cause scarring in the urethra.
This narrows the tube, making urination difficult and increasing the risk of urinary tract infections (UTIs). - Bladder Dysfunction: Chronic infections can sometimes affect bladder function, leading to urgency, frequency, or even incontinence.
Specific STDs and Their Effects
Let’s break down some common STDs and their particular challenges.
Considering your options? We can help! Call us at 96176887676 or book a consultation to get started.
| STD | Primary Fertility Impact | Primary Urological Impact | Key Takeaway |
|---|---|---|---|
| Chlamydia | Epididymitis, reduced sperm quality, potential blockages. | Urethritis, potential urethral strictures, prostatitis. | Often asymptomatic, but highly damaging if untreated. |
| Gonorrhea | Severe epididymitis, orchitis, decreased sperm production. | Urethritis, urethral strictures, chronic prostatitis. | Can cause rapid and severe inflammation. |
| Syphilis | Can affect overall health, indirectly impacting sperm quality; very rare direct fertility impact. | Neurological syphilis can affect bladder control in late stages. | Primarily systemic, but late stages are serious. |
| Herpes (HSV) | Rarely a direct fertility impact; psychological stress can affect sexual function. | Can cause painful sores in the genital/urethral area, leading to difficulty urinating during outbreaks. | More about symptoms and discomfort than fertility damage. |
Protecting Your Health: Prevention and Early Action
Simple Steps for Protection
- Safe Practices: Always use condoms correctly and consistently during sexual activity.
- Regular Screenings: If you are sexually active, especially with multiple partners, regular STD screenings are crucial.
Many STDs show no symptoms early on. - Open Communication: Talk to your partners about their sexual health history and get tested together.
- Seek Care Immediately: If you suspect you’ve been exposed or experience any symptoms (like unusual discharge, pain during urination, or genital sores), don’t delay seeking medical attention.
At Modern Care, we provide confidential and comprehensive sexual health services right here in Antelias, Lebanon.
You can find our clinic location easily on Google Maps.
Frequently Asked Questions
Can STDs cause permanent infertility in men?
Yes, unfortunately, if left untreated, some STDs like chlamydia and gonorrhea can lead to permanent damage to the epididymis or testicles, causing blockages or severely reducing sperm production.
This can result in irreversible male infertility.
Early diagnosis and treatment are key to preventing this.
What are the early signs of an STD in men?
Early signs can vary greatly, and many STDs are initially asymptomatic.
However, common symptoms might include unusual discharge from the penis, painful urination, sores or warts on the genitals, itching, or pain in the testicles.
It’s important to remember that you might not have any symptoms at all, which is why regular testing is so vital.
Is it possible to treat STDs and reverse the damage?
Bacterial STDs (like chlamydia and gonorrhea) are treatable with antibiotics, which can cure the infection and prevent further damage.
However, any scarring or structural damage that has already occurred (like urethral strictures or severe blockages in the epididymis) might not be fully reversible and could require additional urological procedures.
Viral STDs (like herpes or HIV) are not curable but can be managed with medication to reduce symptoms and transmission.
Understanding The Impact of Untreated STDs on Male Fertility and Urological Health is a crucial step toward taking control of your well-being.
Don’t let embarrassment or lack of information put your future health at risk.
Early detection, proper treatment, and preventive measures are your best tools for maintaining both your reproductive and urological health.